As I have become more and more focused on the study of Pelvic Health and the important role it plays in our confidence in socializing, staying active, and intimacy, the more I realize that education is the biggest factor affecting this issue.
Urinary incontinence (UI) is something that is often whispered about, but never fully discussed or understood out loud. So those of us suffering from UI think we are alone….
YOU ARE NOT ALONE!
Studies show that 1 in 4 women report symptomatic pelvic floor disorders, and that 41% of women opt out of exercise because of urinary incontinence. Even more alarming, another study reports that nearly half of female adolescent athletes experience some form of urinary incontinence.
Let’s talk about the bladder, because understanding your body is the first step in learning what can go wrong and how to make changes. The typical adult bladder can hold between 400-600ml of urine. That is a grande latte from Starbucks!
Since we all have a similar amount of storage, why do some of us feel like we have a “small bladder” and can’t get through a day without some sort of bathroom emergency? This is called urinary incontinence: the unintentional passing of urine.
The more common forms of urinary incontinence are Stress Incontinence and Urge Incontinence.
Stress incontinence - leakage due to increased abdominal pressure under stress and weak or dysfunctional pelvic floor muscles, examples such as:
when you cough or sneeze
while exercising
lifting your groceries out of your trunk
Urge incontinence - the uncontrollable urge to pee due to involuntary contraction of the bladder muscles:
as you pull out your keys when you return home from being out
hearing running water
when you see a bathroom sign
WHAT DO I DO ABOUT IT?!?!
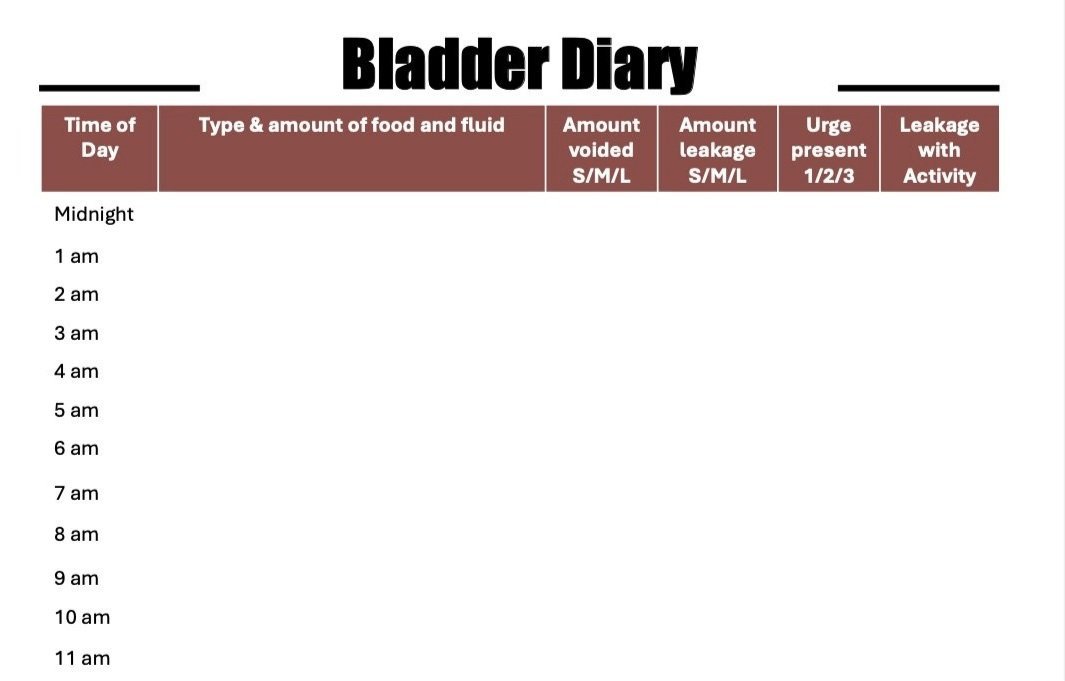
If you want some insight into your own bladder’s patterns, try keeping a bladder diary.
Click this image to open a daily voiding log from HermanWallace.com
A bladder biary is a simple chart which allows you to record the fluid you drink and the urine you pass during the day and night, as well as document if you have urgency (a sudden and intense need to pass urine that cannot be put off) and/or accidental urine leakages.
GREAT! I’VE DONE THE LOG, BUT WHAT DOES IT MEAN?
To help you interpret the data you collect in the bladder diary, I highly recommend finding a physical therapist that specializes in Pelvic Health. This is a vulnerable area of the body and a topic that (shouldn’t be, but) is embarrassing to talk about. First, it’s important to know that a pelvic health therapist understands the awkwardness and is there to support you. Their job is to educate you about your symptoms and diagnosis, inform you about treatment intervention options and together form a plan of care that can get you to your goals.
A bladder diary can provide you and your physical therapist valuable insight into your urinary incontinence and work with you on the appropriate treatment, whether it be changing your bladder habits and/or pelvic floor strengthening exercises.
It has been shown in many studies that Physical Therapy intervention for pelvic floor dysfunction is one of the most effective treatment interventions for those of us suffering from urinary incontinence.
REFERENCES:
Pelvic floor muscle training protocol for stress urinary incontinence in women: A systematic review
The Prevalence of Urinary Incontinence among Adolescent Female Athletes
Prevalence and trends of symptomatic pelvic floor disorders in U.S. women
Effectiveness of Pelvic Floor Muscle Training on Quality of Life in Women with Urinary Incontinence